Surgery
Surgical Repair
The bone surrounding the superior canal is one of the few bones in the body that does not repair itself. As such, the dehiscence will never heal by itself.
As mentioned, some SCDS patients are able to adjust to their symptoms over time. In those cases, it is recommended to keep with symptom management, and have follow-up appointments with an ENT specialist.
For those that have symptoms that severely impact their quality-of-life, surgery is an option to consider.
Finding a Surgeon
When considering surgery, it is important to remember:
- Surgery to repair SCDS is an invasive, extremely delicate operation.
- Recovery typically takes several weeks or months.
As such, it is critical to find a specialist surgeon that is very knowledgeable of SCDS, and has a proven record of successful surgeries.
Types of Surgery
The superior canal is located behind the skull near your ear, and resides underneath the brain's dura (the protective membrane that surrounds the brain). Because of this location, an opening in the skull must be created by the surgeon in order to access the inner ear and repair the dehiscence.
There are two different types of surgeries used in SCDS operations:
- Transmastoid (referred to online as TM)
- Middle Fossa Craniotomy (referred to online as MFC)
TM and MFC have the same types of risks (such as hearing loss), and total recovery time is approximately the same on average.
Your surgeon will recommend which approach to use based on several factors, including the location of the dehiscence.
Transmastoid (TM) Approach
TM surgery is performed behind the ear, and is the least-invasive of the two types of surgeries. It can be performed by an ENT surgeon alone, and is typically considered an out-patient day surgery. The downside to the TM approach is that the surgeon has no direct visualization of the dehiscence.
Middle Fossa Craniotomy (MFC) Approach
MFC surgery is performed by making an opening in the skull above the ear. MFC is a more invasive surgery that requires both an ENT and a neurosurgeon, as the brain dura must be lifted slightly to access the inner ear. However, the MFC approach allows the surgeon to have a complete visualization of the dehiscence.
Types of Repairs
During the surgery -- whether TM or MFC -- the surgeon will repair the dehiscence using one of several methods:
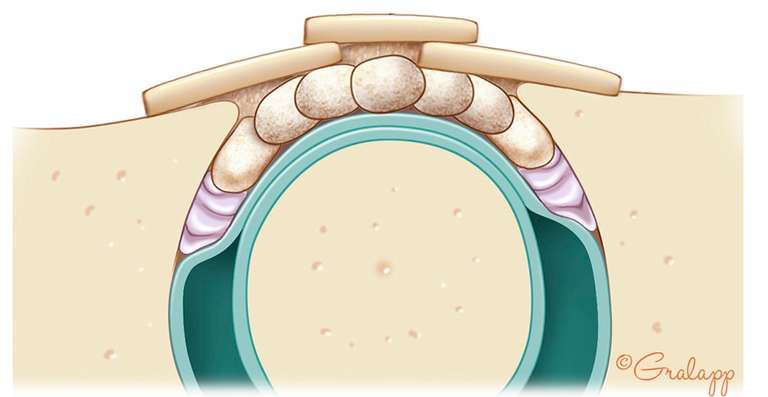
- Plugging - this is where the surgeon plugs the canal completely, closing the canal. This method helps prevent SCDS symptoms from reoccurring long-term.
- The downside is that this reduces or disables the functionality of that canal, which can cause dizziness and balance issues after surgery. However, the brain typically re-adjusts within several weeks or months, and vestibular rehabilitation therapy can assist with the recovery.
- Resurfacing (sometimes called Sealing or Capping) - this type of repair attempts to cover the hole caused by the dehiscence without plugging the canal.
- The advantage to this type of repair is that it can help preserve the function of the superior canal by not disabling it, which can reduce post-operative dizziness. However, resurfacing alone has the risk of the repair material being reabsorbed by the body overtime, which could allow the dehiscence to reappear.
In many cases, surgeons will use both methods to ensure the best long-term results.
Repair Images
Plugging of the superior canal:
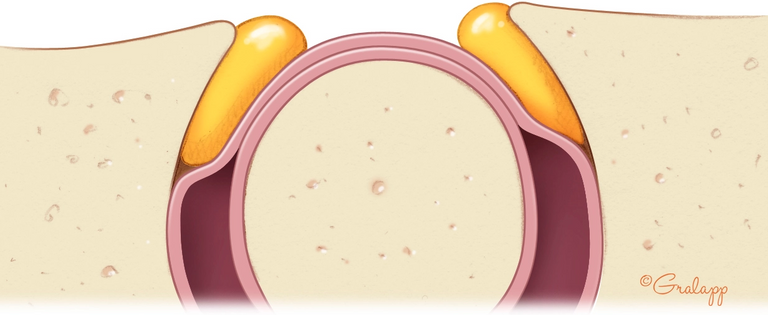
Resurfacing plus plugging of the superior canal: